Translating research into technology
When researchers and medical professionals need to measure a patient’s cerebral and tissue oxygenation, they choose from a variety of tools – positron emission tomography (PET), magnetoencephalography (MEG), electroencephalogram (EEG), computerized tomography (CT), and functional magnetic resonance imaging (fMRI) scans can all provide key data. However, there are a number of drawbacks to current diagnostic tools. These systems are prohibitively expensive. They can have slow response times, low spatial resolution, and be distressingly loud for patients, and they rely on large components that draw enormous amounts of power and are not suited to being manufactured at small sizes. They require access to a heavy external battery or a wall socket, so if movement is required, patients are connected to a fiber optic cable harness that interferes with their freedom of motion.
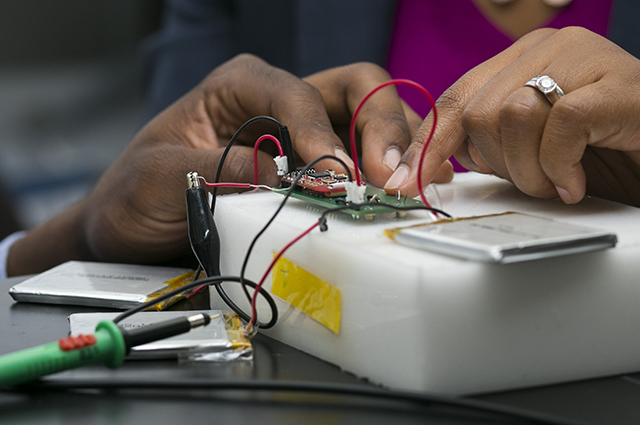
Associate Professor Valencia Koomson and researchers in her Advanced Integrated Circuits and Systems Laboratory in the Department of Electrical and Computer Engineering are developing an innovation that could change the game entirely. The HemoSensis prototype would be the first frequency-domain near-infrared spectroscopy (fdNIRS) device to measure cerebral and tissue oximetry in a compact form factor – untethering patients from bulky, power-hungry instruments and providing a lower-cost, noninvasive monitoring tool at the bedside.
Without oxygen, tissue and brain cells quickly begin to die. Severe brain damage and death can occur after just a few moments of oxygen deprivation. The HemoSensis device could help doctors and researchers better monitor vulnerable premature babies’ health, assess traumatic brain injury for patients in hospital intensive care units, or diagnose injuries in combat zones or low-resource environments where drawing large amounts of electricity or installing heavy, expensive equipment is out of reach.
The proposed prototype measures less than one cubic centimeter and requires a very small amount of power. It uses low-cost, solid-state optical devices and a system-on-chip platform. “The core processing unit is a custom-designed fdNIRS microchip that combines opto-electronic interface drivers and complex signal processing circuitry with detection on a single 5mm x 5mm piece of silicon,” says Koomson. Additional benefits of the proposed prototype include a higher signal-to-noise ratio (the ratio that compares the strength of a signal carrying information to the strength of interference), the ability to measure at selective depth sensitivity rather than only measuring intensity, and improved spatial resolution.
Koomson wants to produce a scalable product that could be easily incorporated across multiple platforms and create an entire new class of wearable oximeter instruments. With funding provided by a National Science Foundation (NSF) Partnerships for Innovation Technology Transfer grant, Koomson’s team is developing the initial proof-of-concept device now. Their work builds on the foundation set by Koomson’s earlier research, funded by a 2011 NSF CAREER Award, on a new class of imaging sensors that can characterize biological structures at minimal disruption for patients.
Koomson’s team is making good use of Tufts’ strong footprint in entrepreneurship, involving colleagues from across the university and beyond. To name just a few Tufts partners, they plan to collaborate with the Tufts Entrepreneurship Center, Tufts Gordon Institute, the M.S. in Innovation and Management program, the Office of Technology Licensing and Industrial Collaboration, and Tufts Clinical and Translational Science Institute. The research team participated in the NSF Innovation Corps Spark Program, hosted at MIT this summer, to further explore the potential applications of the new technology.
Koomson has her eye on the future. “Our device addresses a medical need that’s not currently met by existing technology,” she says. “I’m looking forward to advancing our work in frequency domain tissue spectroscopy techniques and reaching a significant new milestone in the development of point-of-care diagnostic tools.”
This research is funded by National Science Foundation award 1919038, “PFI-TT: A Noninvasive Biological Research Tool for Measurement of Tissue and Cerebral Oxygenation.”
Department:
Electrical and Computer Engineering