Going to great wavelengths
By Kristin Livingston, A05
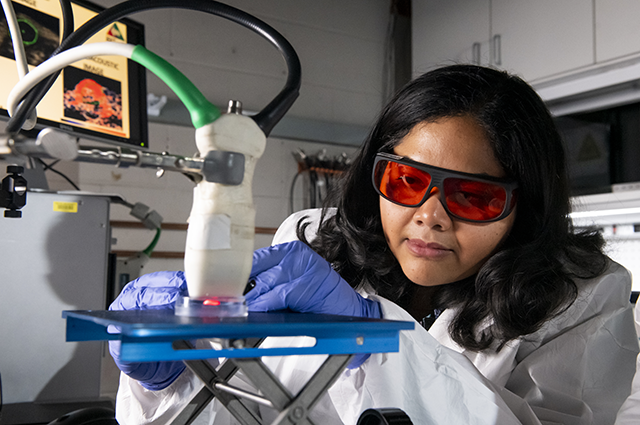
“It’s like lightning and thunder.” That’s how assistant professor of biomedical engineering Srivalleesha Mallidi describes the photoacoustic imaging technology that she uses for cancer research in her Integrated Biofunctional Imaging and Therapeutics Laboratory at Tufts—also known as the iBITLab.
The lab focuses on using light and sound energy to image tumors non-invasively in their early stages. Mallidi’s research utilizes a photoacoustic phenomenon where a short pulse nanosecond laser light generates sound waves around the tumor for detection by ultrasound. Different light wavelengths show the region’s vascular density and oxygenation to better understand the tumor’s properties. When patients are injected with a contrast agent that can specifically localize the tumors, the use of photoacoustics can then also identify the margins of the tumor, helping surgeons save as much healthy tissue as possible. Mallidi is collaborating with Massachusetts General Hospital to test this research on oral cancer patient samples and has so far observed positive results in preclinical models. The use of an ultrasound machine versus an MRI or CT scanner is also a cost-effective boon and more widely available to patients.
The iBITLab is also working on developing algorithms to predict treatment response at early time points, particularly looking at vascular and hypoxia surrogate markers. “The main way tumors get nutrients is through these blood vessels. However, due to excessive growth, tumors also have hypoxic areas,” Mallidi explains. Chemotherapy and radiation don’t work in a hypoxic environment, so she is researching how to predict, with imaging biomarkers, whether a patient will respond to these therapies or not—saving valuable time, understanding resistance to therapy, and reducing overexposure to systemically toxic therapies.
Guiding surgical methods, predicting therapeutic response, and designing effective therapeutic strategies are the core of Mallidi’s work in the iBITLab. But the crown jewel has become her recent work on image-guided photodynamic therapy, or PDT, a light-based therapy in which wavelengths of light irradiate, and kill, cancer cells loaded with a light-activated cytotoxic drug called a photosensitizer.
“PDT has been around for a long time, at least 20 years,” Mallidi says, “but hasn’t caught up to mainstream therapy, despite showing great promise.” When PDT was introduced, patients had significant photo-toxicity: for example, when a photosensitizer was injected, any sun exposure was toxic. But today, tumor localization is possible via encapsulation in nanoparticles. Combined with photoacoustic imaging to understand drug delivery, designing dosimetry and monitoring treatment response, better treatment strategies are on the horizon.
At the 2019 International Photodynamic Association World Congress, Mallidi was honored with the Early Investigator Award in recognition of her exceptional research and clinical translation of PDT. “It really excites me,” she says. “I’m an electronics engineer by training and my PhD focused on building imaging systems.” Before beginning her post-doctoral work at Harvard, she had limited knowledge of cancer research and nanotechnology. But, like everyone, Mallidi’s family was also affected by cancer. “I wondered, ‘Can we do something about this?’”
“Now that I’m at Tufts, where I’m able to integrate all of my research, I’m motivated every day to get up, deeply think about the problem, and find new solutions.”
Department:
Biomedical Engineering