Breath of fresh air
By Lynne Powers
In areas hit particularly hard by the COVID-19 pandemic this spring, medical workers faced a grim scenario: there were more critically ill patients than there were ventilators available. Some patients with severe cases of COVID-19 develop acute respiratory distress syndrome (ARDS), in which inflammation of the lungs interferes with the ability to absorb oxygen and expel carbon dioxide. Ventilators can help keep patients alive by mechanically moving air into and out of the lungs. Hard-hit hospitals faced waves of patients struggling to breathe and suffering from ARDS, which forced doctors and respiratory therapists to grapple with life or death choices: which patients would receive ventilator support? The race was on to increase the global supply of ventilators – quickly and safely.
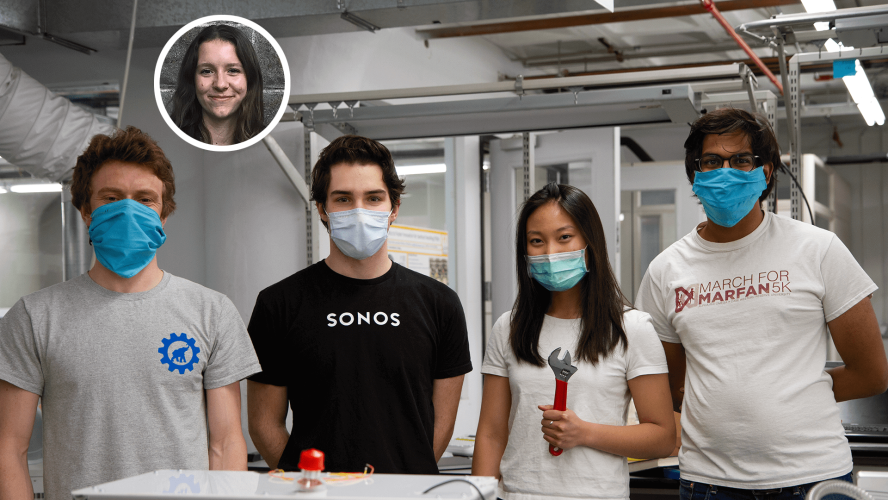
A group of Boston-based entrepreneurs and engineers saw the urgent need for new ventilator designs that could be produced efficiently at low cost without sacrificing safety and effectiveness. With a new nonprofit rapidly taking shape, the Ventilator Project team reached out to colleagues across sectors, including faculty at Tufts School of Engineering. Dozens of volunteers joined the project within days, and their numbers would eventually swell to over 200. Among their ranks were five Tufts students and alumni: Shounak Bose, EG20, Olive Garst, E21, Klare Hu, E21, Christopher Markus, E20, and Courtland Priest, E19.
The team had a shared goal: to produce a low-cost, sustainable ventilator prototype that would receive Emergency Use Authorization, a federal designation that allows the U.S. Food and Drug Administration (FDA) to authorize new medical technologies and treatments on an advanced timeline during public health emergencies. The group followed the typical engineering process of (1) design, (2) build, (3) test, and (4) iterate, but moved at lightning speed – a process that might normally take months now took days.
A team effort
Modern ventilators are complex computerized machines controlled by microprocessors, which bring together engineers from across a wide array of disciplines. Electrical engineering majors Olive Garst and Christopher Markus worked on firmware and electrical engineering. Throughout the spring, “I pivoted from mainly working on analog alarm circuitry to designing the system controller printed circuit board to writing firmware to a lot of debugging,” said Garst. Markus, meanwhile, was the lead firmware engineer for the project and was tasked with figuring out how systems work together, writing code, and building and managing the firmware engineering team.
Courtland Priest had just completed his BS in mechanical engineering in December 2019. “I had a strong desire to do something to directly assist the pandemic relief effort,” he said. “This project came along and provided me an avenue to do just that.” He served as a lead mechanical design engineer, which meant working on everything from hardware integration to mechanical component design, from communicating with suppliers to supervising engineering interns.
Likewise, mechanical engineering major Klare Hu quickly found herself filling multiple roles. She saw the project’s early need for electrical engineers and nimbly shifted across teams to become a lead electrical engineer. She implemented electrical circuits, designed an Arduino shield board for sensors and solenoids, and filled out failure modes and effects analysis documentation.
Shounak Bose was finishing his MS in biomedical engineering when the opportunity arose to lend a hand. “We’ve generally maintained about 25 on-site team members and over 100 remote volunteers,” he said, primarily with college students and young professionals on-site and experienced industry professionals providing remote guidance and troubleshooting. Bose was on the project’s quality assurance (QA) team, which facilitated the prototype’s testing procedures and worked to find bugs. The QA process holds a particularly key role in designing ventilators, which, as life-critical systems that breathe for patients, must be highly reliable and tested to within an inch of their mechanical lives.
The Jumbo effect
The students’ background from the School of Engineering prepared them for the intense work. Garst highlighted her project-based classes at Tufts for building a strong foundation in hardware, while team-based work like junior-year design projects eased her transition into a larger scale project and a start-up environment’s constant communication. Markus praised Junior and Senior Design too, saying that the classes taught him to “work on a team and work within requirements you’re given. With everything moving so quickly and with massive lists of requirements from the FDA, we had to be comfortable with ambiguity.” Priest said his technical background and flexibility learned at Tufts meant that he was able to slot in wherever he was needed, including project management roles.
“Tufts had given me the ability to adapt easily across different engineering disciplines,” said Hu, a mechanical engineer by training who became a lead electrical engineer on the project. “While I was working with the Ventilator Project, I was reminded a lot of the hands-on experience I had in [Lecturer] Brandon Stafford’s class, ME43 Electronics for Mechanical Engineers. Working at TVP reminded me of the atmosphere in the Nolop Makerspace, where people work alongside each other to solve hard problems.”
Bose, too, was grateful for the foundation he had built at Tufts. “My lab research in the Department of Biomedical Engineering gave me hands-on experience and data analysis skills, which helped me with designing and evaluating tests for ventilator performance,” he said. Coursework had familiarized him with the design, regulatory, and testing processes for the medical device industry.
While Massachusetts experienced its spring surge in novel coronavirus cases, the Ventilator Project team reported to work both remotely and at the project’s offices in Boston’s Seaport District. The volunteers understood the urgency of the need. “I was driven to volunteer because the Ventilator Project felt like a way to help potentially save lives,” said Garst. Both Garst and Bose returned to Boston to work on the project. Priest often stayed in the project’s downtown hostel, and Markus volunteered full time while finishing the final semester of his senior year at Tufts.
The way forward
The unit that the team developed, called AIRA, could potentially be produced at a fraction of the cost of traditional ventilators. Following a busy spring and early summer, the Ventilator Project shipped three units to an independent testing agency – the first step in the process of achieving FDA Emergency Use Authorization status. With the testing process now complete, the Ventilator Project is awaiting the final decision from the FDA this fall.
“We have been extremely impressed with everyone, especially the students from Tufts University,” said Tyler Mantel, CEO and founder of the Ventilator Project. “When they could have chosen to sit at home and stay put, they instead decided to work 40-hour weeks to create a ventilator for those who need it. Without their contributions, we would be nowhere near as far as we are today.”
As for the Tufts team members, Garst and Hu returned to Tufts this fall for their senior years, while Markus began his MS in computer engineering. Priest started a new job as a project engineer at Aerofit LLC. Several students are still consulting with the Ventilator Project, and Bose stayed on as a policy analyst while he seeks full-time opportunities in the medical device industry.
The Tufts students and alumni look back with pride on their experiences this spring and summer. “I learned so much within the span of three months,” said Hu. “It was amazing to witness the synergy of a group of passionate people turn into life-changing products.”