Tissue healing after a heart attack
Tufts University engineers have developed new, non-destructive techniques to evaluate tissue healing following a heart attack. These techniques, described in a paper recently published in Nature Scientific Reports, could be used to evaluate current treatments for aiding cardiac repair and to provide a basis for evaluating heart disease progression.
Every year, about 735,000 Americans have a heart attack. Of these cases, 525,000 are a first heart attack.* After a heart attack, or myocardial infarction, the body quickly attempts to replace damaged cardiac tissue with new collagen scaffolding to provide support to withstand the forces associated with a normal heartbeat. The body can sometimes overbuild this scaffolding, or extracellular matrix (ECM), or expand the remodeled ECM into heart tissue not initially adversely affected by the heart attack. The altered heart tissue resulting from ECM remodeling is often responsible for functional deterioration, leading to heart failure.
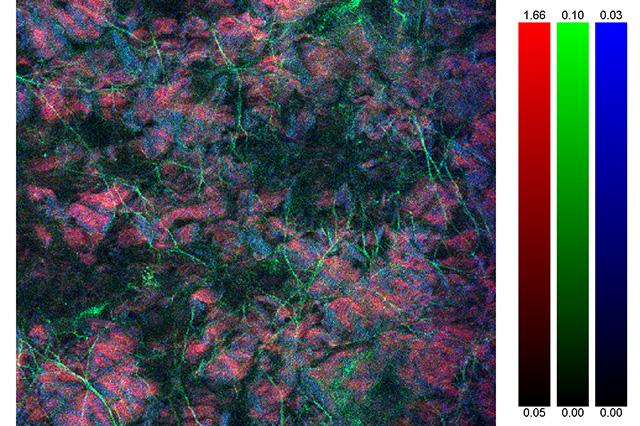
Though scientists have studied some elements of how remodeled tissue structure affects function following heart attack, little is understood about the relationship between ECM composition of the scar tissue and its mechanical properties in the earliest stages of remodeling. By using a process called decellularization—the removal of cells from the heart tissue structure—and pairing this with 3D multi-photon microscopy, the tissue’s mechanical properties and structure remains intact and can be studied. As a result, the Tufts biomedical engineering team has uniquely identified structure-function relationships specific to the myocardial ECM. Specifically they have found that the ECM that is newly remodeled/deposited, following infarction, is weaker than healthy tissues, most likely due to alterations in the chemical connections within and between fibers called “crosslinks.” This weaker ECM may be contributing to the expanding scar by adversely signaling cells in the remodeling tissue to continue to make more ECM.
The team of Tufts researchers included Kyle Quinn, Kelly Sullivan, Zhiyi Liu, Zachary Ballard, Christos Siokatas, Associate Professor Irene Georgakoudi, and Associate Professor Lauren Black.
Read the full paper in Nature Scientific Reports.
* Source: http://circ.ahajournals.org/content/early/2014/12/18/CIR.0000000000000152
Department:
Biomedical Engineering